DEADLY DECISIONS: Health care secrecy in Arizona
How did your country report this? Share your view in the comments.
Diverging Reports Breakdown
DEADLY DECISIONS: Health care secrecy in Arizona
A Tucson surgeon hit with a wrongful death verdict is again shining a spotlight on health care secrecy in Arizona. At least 13 patients died under Dr. Jeffery Monash’s care within six years, with five of those deaths in only six months. The Arizona Medical Board is the state’s watchdog of physicians — the protector of patients. The board received about 1,200 complaints against Dr. Monash, but these complaints are not made public. 13 Investigates found the deck is stacked against the public knowing about questionable doctors. The first part of this story is in the player above. Part II can be watched below. The second part of the story can be seen on 13 News at 10 p.m. and 11 p. m. ET on Thursday, February 14. The third and final part is on Friday, February 15 at 10 a.m and 11 a. M.E. on Saturday, February 16 at 9 a.M. and 9 p.S. on the same channel.
13 Investigates answers the question of who’s responsible for overseeing bad care and why the public is often left in the dark.
13 News’ Valerie Cavazos has reported that at least 13 patients died under Dr. Jeffery Monash’s care within six years, with five of those deaths in only six months.
The first part of Valerie’s newest story is in the player above. Part II can be watched below.
A Tucson surgeon hit with a wrongful death verdict is again shining a spotlight on health care secrecy in Arizona.
Monash has admitted he defined “surgeon burnout” for years, yet he continued to perform surgeries.
Monash told 13 News he did nothing wrong and disputes he was responsible for all but one of the deaths.
We wanted to know who’s overseeing all this and what’s being done.
A STACKED DECK
In the process, 13 Investigates discovered the deck is seriously stacked against the public knowing about questionable doctors.
The Arizona Medical Board is the state’s watchdog of physicians — the protector of patients.
The Board primarily relies on public complaints to launch investigations.
Dr. Barry Weiss, a professor at the University of Arizona College of Medicine, who served on the Arizona Medical Board in the 1990s, talked with 13 News.
“The board can’t take action about things they never heard of. Somebody has to report it and then they will investigate,” he said.
Two attorneys, Michael McNamara and Amy Hernandez, filed complaints after two of Dr. Monash’s patients died in 2020.
Both raised serious red flags alleging serious mental impairment from chronic drug use and severe insomnia that cost more than a dozen patients their lives.
PREVIOUS DEADLY DECISIONS STORIES
“They’ve had all that information since early 2020,” said McNamara.
Both attorneys asked the board to investigate, and both argued Monash’s license should be suspended.
On average, it takes less than a year (252 days) to complete a case.
But McNamara said more than five years later, his complaint is still an open investigation with no end in sight.
“That’s kind of strange,” Weiss said. “That was not my experience on the board. If it’s taking years to evaluate a case, that puts the public at risk because a doctor who may be practicing inappropriately, nobody might know it for a couple of years.”
Regarding Hernandez’s complaint, earlier this year, the Arizona Medical Board reprimanded Monash, saying he provided substandard care.
He’s appealing it, so that means the disciplinary action will not be made public until it’s resolved.
PRIVACY RESTRICTIONS
(Gray Media)
13 Investigates asked the Medical Board leadership for an on-camera interview and was told by law they can’t grant that because of privacy restrictions and would only answer general questions through email.
This means we can’t get answers on specific doctors or cases.
Board leadership explained in an email that, in general, some cases take longer to investigate because of their complexities, legal delays, and staff turnover of longtime investigators.
To put their caseload into perspective, there were 25,000 licensed MD’s in Arizona in 2019, and the board received about 1,200 complaints.
But as 13 Investigates discovered, these complaints are not made public.
Hernandez said, “Unless there’s a formal discipline that becomes public, the patients don’t stand a chance of finding out.”
There have been 5 other complaints against Dr. Monash since 2009. The board dismissed all of them.
Hernandez filed one of them in 2016 after the death of one of his patients.
The family sued, and the case ended in a settlement.
Monash admitted “negligence” in a June 2017 letter sent to Hernandez by his attorney and also to 13 Investigates during a recent interview.
Monash said, “There was one patient, Michelle Halderman, that you mentioned that I did think I made an error on, and I didn’t argue it. And you know what, I’m human.”
DISMISSED COMPLAINT
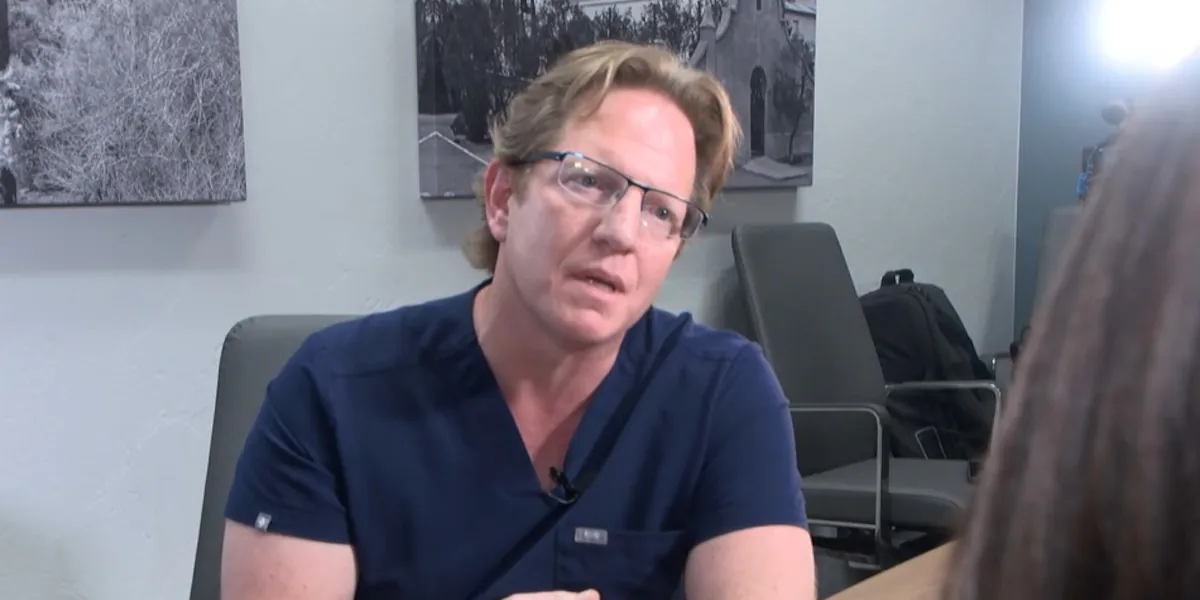
Dr. Jeffrey Monash. (13 News)
So it came as a shock to Hernandez when the board dismissed her complaint — no details given.
Hernandez said, “If their duty is to protect the public and this doctor has said I was negligent and made a mistake in this case, why then there seems to be no reason that I can come up with that they would then dismiss it.”
McNamara said, “I think all 13 of these deaths could have been prevented.”
McNamara asked for the board to investigate after he discovered a slew of red flags that he charted and presented to the jury in Dr. Monash’s trial.
What’s charted around the 13 patient deaths is important.
The chart lists serious injuries, medical and behavioral incidents, and hospital peer reviews.
There are seven deaths charted in the span of a year from 2014 to 2015.
DRUG USE, INSOMNIA, AND DEPRESSION
(Randy Tisor / Stars and Stripes)
Around that time, court records show Monash admitted to chronic drug use, severe insomnia, sleeping only a few hours a night, and depression.
In 2016, attorney Amy Hernandez filed a wrongful death lawsuit.
Hernandez said, “As we settled the case, I did report and I was required to by statute and in that specific case, Dr. Monash did admit guilt.”
A sheriff’s document in 2017 shows he threatened suicide.
From 2018 to 2020, Monash admitted he was going through a difficult divorce.
A court-ordered clinical psychologist, Dr. Holly Joubert, testified that Monash appeared to be “manifesting anxiety, paranoia, poor concentration, delusions, difficulty with perceptions, it can lead to even psychosis, trouble making decisions.”
McNamara pointed to court records showing Monash tested positive for marijuana the same day he performed three surgeries in 2019.
io (WTVG)
That same year, he admitted to self-medicating with unprescribed Percocet, which is illegal.
McNamara documented for the jury several serious incidents involving extreme behavior.
“Numerous very bizarre incidents that occurred around this time involving things like emotional outbursts at work, performing a surgery that was several surgical procedures that had very unusual or bizarre events that did not result in serious patient injury ultimately, but might have. They’ve had all that information since early 2020, and it’s now 2025,” said McNamara.
Both McNamara and Hernandez question what exactly the board knows.
They say physicians, by law, have to self-report serious issues like substance abuse and mental impairment.
“Yes, physicians are supposed to self-report problems that are on that list of things they have to report,” said Weiss.
But Hernandez believes the board shouldn’t rely on physicians to self-report.
“That goes against what is our human nature, which is our self-interest,” said Hernandez.
REQUIRED REPORTING
(Live 5/File)
Weiss said medical staff, physicians, nurses, administrators, have a statutory responsibility to report questionable doctors.
Weiss said, “If there’s a physician who’s repetitively not practicing well and nobody reports it, it’s a lot of people’s fault not reporting it.”
And they can face disciplinary action.
McNamara has documented about two dozen hospital peer reviews since 2012.
Weiss said, “If something’s coming to the attention of a hospital peer review committee over and over and over and over and over, yeah, that is a red flag.”
Monash eventually resigned in 2020 after three more deaths.
He stated the reason in his resignation letter — “surgeon burnout” for years and he needed to step away for the safety of his patients.
He wrote, “Not only is it your duty to do what is safe for patients and the hospital, it is mine.”
None of this, including the reason for his resignation, appears on the Arizona Medical Board’s website.
But what has now appeared as of June 2025 is the AZ Medical Board’s Letter of Reprimand for “substandard care” relating to Amy Hernandez’s 2020 complaint.
Hernandez offers this advice.
“You need someone with you,” said Hernandez. “You need an advocate. They’re a second set of eyes. They’re the second set of ears. You just have to be diligent. And so that’s what I say, patients don’t stand a chance. There’s a lot you don’t get to know, by law.”
Monash still has his Arizona medical license.
He has continually argued he’s done nothing wrong.
You can submit your breaking news or weather images here .
Copyright 2025 13 News. All rights reserved.
Source: https://www.kold.com/2025/06/20/deadly-decisions-health-care-secrecy-arizona/
