Kennedy says health insurers promise to change prior authorization process
How did your country report this? Share your view in the comments.
Diverging Reports Breakdown
Kennedy says health insurers promise to change prior authorization process
Prior authorization is a cost-cutting tool used by health insurers. It requires them to sign off on tests, procedures or drugs before patients can get them. The insurance tactic drew renewed attention last year after the fatal shooting of Brian Thompson, the CEO of UnitedHealth’s insurance arm. About 1 in 6 insured adults say they’ve had prior authorization problems, according to a survey from KFF, a health policy research group. The changes will be implemented across private insurance, Medicare Advantage and Medicaid, trade group says.. Health insurance companies have made similar commitments to fix prior authorization in the past, a fact Kennedy and Dr. Mehmet Oz, administrator of the Centers for. Medicare & Medicaid Services (CMS), acknowledged at a media event Monday. In 2018 and again in 2023, health insurance companies made commitments to reform prior. authorization, Oz said.
Prior authorization is a cost-cutting tool used by health insurers that requires them to sign off on tests, procedures or drugs before patients can get them.
The insurance tactic drew renewed attention last year after the fatal shooting of Brian Thompson, the CEO of UnitedHealth’s insurance arm, in New York City.
Patients and doctors say prior authorization creates too many roadblocks, forcing people to wait days or weeks for needed treatments or denying them altogether.
About 1 in 6 insured adults say they’ve had prior authorization problems, according to a survey from KFF, a health policy research group.
Kennedy said a number of large insurance companies — including Blue Cross Blue Shield Association, Cigna, Elevance Health, GuideWell, Humana, Kaiser Permanente and UnitedHealthcare — pledged to make the changes, which will be implemented across private insurance, Medicare Advantage and Medicaid.
AHIP, a health insurance industry trade group, said the changes could benefit 257 million people in the United States.
Experts stressed, however, that prior authorization isn’t going away.
It’s “going to streamline it in some incremental ways only,” said Dr. Adam Gaffney, a critical care physician and assistant professor at Harvard Medical School.
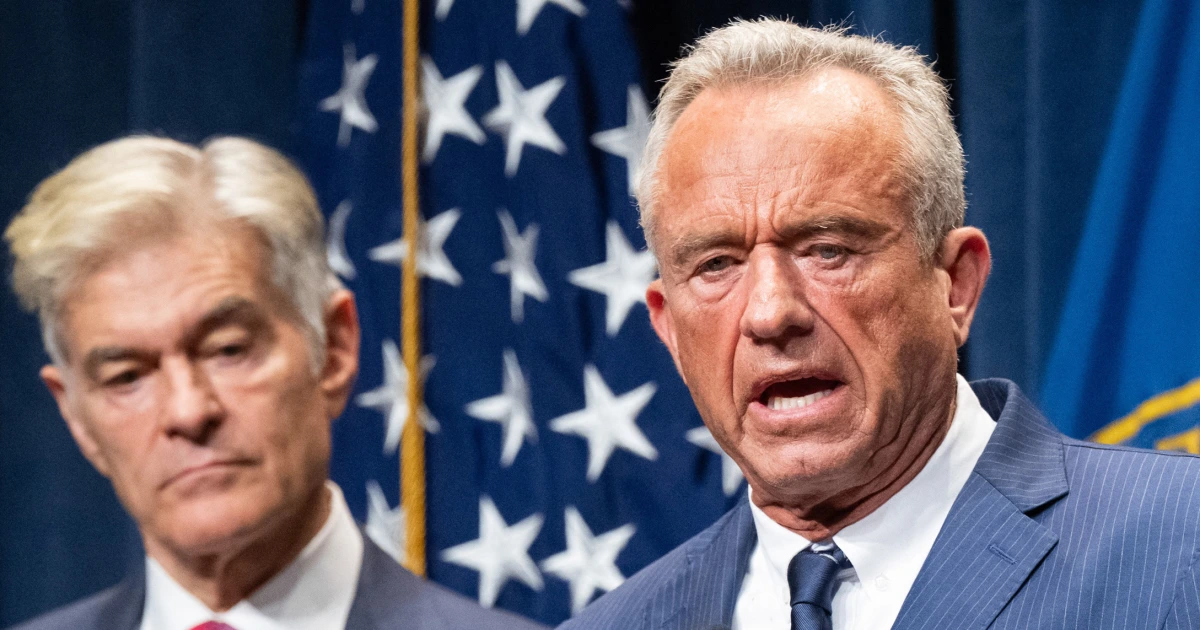
Health insurance companies have made similar commitments to fix prior authorization in the past, a fact Kennedy and Dr. Mehmet Oz, administrator of the Centers for Medicare & Medicaid Services (CMS), acknowledged at a media event Monday. In 2018 and again in 2023, health insurance companies made commitments to reform prior authorization, Oz said, but many failed to implement such reforms.
Asked what’s different this time, he said, “There’s violence in the streets over these issues,” alluding to the shooting of Thompson.
AHIP — formerly America’s Health Insurance Plans — detailed the steps health insurance companies committed to in a news release earlier Monday.
Starting next year, if patients switch insurance plans while they are receiving treatment, their new plans will honor the existing prior authorizations for similar care for up to 90 days. In addition, next year, insurers will need to provide easier-to-understand explanations when they deny authorizations and offer guidance about how to appeal.
Insurers have pledged to have medical professionals review all authorization denials, though AHIP said that is something that insurers say they already do.
Insurers have also committed to streamline the prior authorization process by making it easier to submit requests online by 2027. At least 80% of electronic requests will be answered in real time by 2027, AHIP said.
Plans may also reduce the number of medical services subject to prior authorizations in certain cities or states — though specific commitments about what that might include were lacking.
Chris Klomp, who leads the Medicare program at CMS, said the agency would like insurers to roll back prior authorization requirements for common services, including colonoscopies, cataract surgery and childbirth.
Kennedy also said CMS is working with insurers to make it easier to get prior authorization for diagnostic imaging, physical therapy and outpatient surgery.
Gaffney criticized the pledges, saying insurers have had decades to change their practices.
“Talk is cheap,” Gaffney said. “More fundamental reform will be needed to address the ubiquitous barriers to care imposed by insurance firms.”
Kaye Pestaina, director of the program on patient and consumer protection at KFF, said some of commitments could have direct impacts on patients, such as honoring existing prior authorizations for three months after patients switch insurers.
