Recent Policy Proposals Could Weaken the Reproductive Health Safety Net as More People Become Uninsured
How did your country report this? Share your view in the comments.
Diverging Reports Breakdown
Recent Policy Proposals Could Weaken the Reproductive Health Safety Net as More People Become Uninsured
The 2025 Federal Budget Reconciliation Law is projected to result in significant growth in the uninsured rate over the next decade. Among women of reproductive age on Medicaid, 8 million (36%) are eligible through the ACA coverage expansion and could be at risk for losing their coverage due to the new work and eligibility verification requirements. The Trump Administration is currently withholding Title X family planning funds from close to 300 family planning clinics and proposed to eliminate the program altogether in their FY2026 budget. The Supreme Court ruling in Medina v. Planned Parenthood has enabled states to exclude Planned Parenthood clinics from their Medicaid provider networks. This change, combined with the withdrawals of Title X funds to several non-profit organizations and Planned Parenthood grantees, and the rise in uninsured will place additional pressure on an already fragile reproductive health safety net. The Congressional Budget Office estimates that over the course of 10 years, the new law will increase the number of people without health insurance by 10 million because of the changes to Medicaid and Affordable Care Act (ACA) Marketplace coverage.
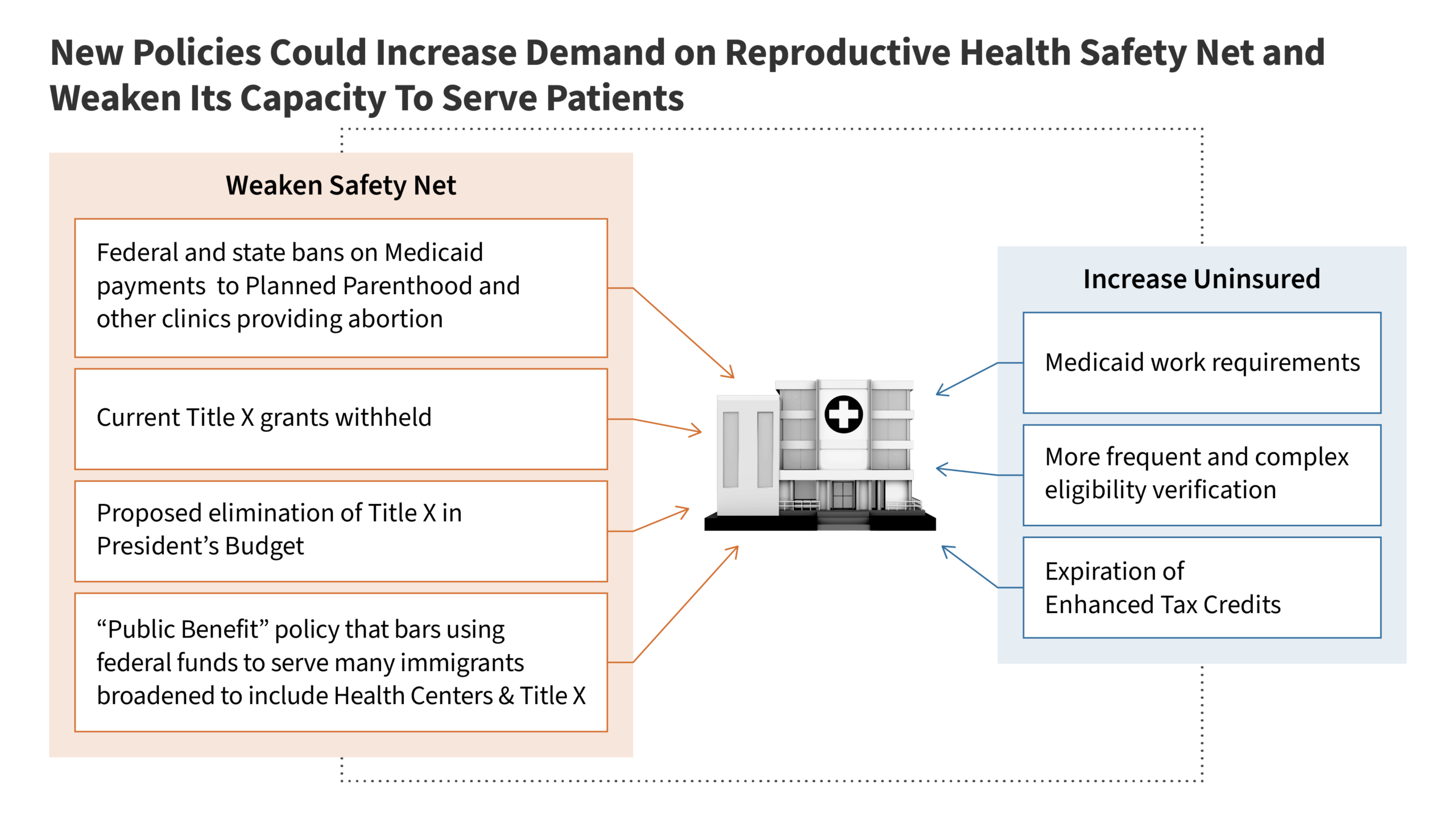
Multiple policy changes resulting from Congressional action, Trump administration efforts, and a Supreme Court decision will significantly weaken the family planning safety net at a time when there will be increasing demand for safety-net providers in every state due to growth in the number of uninsured Americans. The 2025 Federal Budget Reconciliation Law is projected to result in significant growth in the uninsured rate over the next decade through loss of Medicaid and Affordable Care Act (ACA) Marketplace coverage. Among women of reproductive age on Medicaid, 8 million (36%) are eligible through the ACA coverage expansion and could be at risk for losing their coverage due to the new work and eligibility verification requirements.
The 2025 Budget Reconciliation law also bans federal Medicaid payments to Planned Parenthood clinics for one year; however, this provision is currently blocked for all Planned Parenthood members by a federal district court order. The program is the largest source of public financing to Planned Parenthood and also affects a subset of other family planning clinics that also offer abortion services. Among women on Medicaid who obtained family planning services, 11% (about 1 million) got care at a Planned Parenthood in 2021 and the vast majority of them (85%) got contraceptive services.
The Supreme Court ruling in Medina v. Planned Parenthood has enabled states to exclude Planned Parenthood clinics from their Medicaid provider networks. In the past decade, at least 14 states have used state-level policies or sought federal permission to block the provider from participating in their state Medicaid programs, though they have often been blocked by court action, until this ruling.
The Trump Administration is currently withholding Title X family planning funds from close to 300 family planning clinics and proposed to eliminate the program altogether in their FY2026 budget. The federal Title X program provides grant funding to nearly 4,000 clinics to deliver free and low-cost family planning care to people with low incomes.
Combined, these actions could result in closures and cutbacks in contraceptive care and STI services when there will be a greater need for free or low-cost reproductive health care.
Introduction
Over the next few years, a confluence of policy changes at the federal level will significantly weaken and challenge the family planning safety net of publicly supported health centers and clinics. The clinics that currently serve millions of women with low incomes will simultaneously face greater demand for reproductive health care as a growing number of uninsured people turn to the safety net for free or reduced cost care. The reproductive health safety net includes Federally Qualified Health Centers, Title X clinics, Indian Health Service and Rural Health Clinics, state and local health departments, and Planned Parenthood clinics. The impact of the 2025 Federal Budget Reconciliation Law is projected by the Congressional Budget office to increase the number of people uninsured by 10 million over the next decade, and the sunsetting of supplemental ACA premium tax credits at the end of this year could lead to millions more uninsured. The new law would also eliminate Planned Parenthood’s eligibility to receive federal Medicaid funds provider for one year; however, this payment ban is temporarily blocked by court order. This change, combined with the withdrawals of Title X funds to several non-profit organizations and Planned Parenthood grantees, and the rise in uninsured will place additional pressure on an already fragile reproductive health safety net.
Each of these changes alone place considerable pressure on the family planning safety-net and taken together, could result in major access problems not just for low-income people seeking contraceptive care, STI screening and treatment, and other preventive services, but others who rely on this network in every state in the country. This brief details the likely impact of these different actions on the family planning safety net and its ability to provide reproductive health care to millions of people across the nation (Figure 1).
The 2025 Budget Reconciliation Law
The 2025 Federal Budget Reconciliation Law, signed into law on July 4, 2025, will have major impacts on the uninsured rate, as well as the reproductive health safety net that was designed to serve individuals who have low incomes or who do not have health insurance.
Growth in Uninsured Patients
The 2025 Budget Reconciliation Law places additional requirements on Medicaid eligibility that are projected to lead to a major increase in the number of uninsured, a population that relies on the health care safety net for their reproductive health care. The Congressional Budget Office (CBO) estimates that over the course of 10 years, the new law will increase the number of people without health insurance by 10 million because of the law’s changes to Medicaid and the Affordable Care Act (ACA).
Medicaid expansion has provided an important eligibility pathway for low-income women of reproductive age. Today, 8.0 million women ages 19-49 (36% of reproductive age women enrolled in Medicaid) qualify through the expansion alone (Figure 2). The 2025 Federal Reconciliation Law would require Medicaid enrollees who qualify through ACA expansion to work or look for work, but exempts parents with dependent children under age 14. KFF research shows that most adult women covered by Medicaid meet work requirements or would qualify for an exemption, but many would be at risk of losing coverage because of the administrative burden related to reporting requirements. Although work requirements are the largest source of coverage loss, all states are estimated to experience reductions in Medicaid enrollment due to additional administrative hurdles related to eligibility determination, verification, and the frequency of renewals required by the new law.
This erosion in coverage could be compounded by the expiration of the enhanced premium tax credits for ACA Marketplace enrollees at the end of 2025 if Congress does not act to extend them.
Faced with higher costs or challenges getting reproductive care, uninsured women could decide to stop using contraception because they cannot afford it or switch to a less effective method, which could result in an increase of unwanted pregnancies and a loss of reproductive autonomy. The 2024 KFF Women’s Health Survey found one in five uninsured women of reproductive age has had to stop using a birth control method in the past 12 months because they couldn’t afford it, a rate that is four times greater than those with Medicaid (5%) or private insurance (2%).
Medicaid and Planned Parenthood
The most immediate impact of the 2025 Budget Reconciliation Law is the prohibition of federal payments for one year to certain family planning providers that receive at least $800,000 in Medicaid revenue and are affiliated with providers that also offer abortion services. This narrow definition affects all Planned Parenthood clinics as well as two other networks of clinics in Massachusetts and Maine and will be a major economic blow to these clinics that rely heavily on Medicaid as a source of financing for care as well as the over one million women on Medicaid who rely on them for their care. This provision is being challenged by Planned Parenthood and Maine Family Planning and is currently blocked for all Planned Parenthood members as the case moves through the courts.
The federal Medicaid program pays 90% of all family planning services and supplies, and states pay 10%. This is considerably higher than the federal match that states receive for most other services. If the cases challenging the payment ban do not ultimately succeed, it will be difficult if not impossible for states to fill the gap in the loss of funds.
The largest source of financing to Planned Parenthood is the Medicaid program, which reimburses clinics for services provided to enrollees in the same way that it pays private doctors and hospitals. In 2021, one in ten (11%) Medicaid enrollees received their family planning services at a Planned Parenthood clinic and 85% of them received contraceptive services. The share of Medicaid enrollees served by Planned Parenthood varies considerably from state to state (Figure 3).
Federal Medicaid funds do not pay for abortion care, except under very limited circumstances (rape, incest, life endangerment of the pregnant person), because of the Hyde Amendment. Nonetheless, over the last decade, many states have made efforts to ban Planned Parenthood from participating in Medicaid because they also offer abortion services. Federal Medicaid law permits any willing and qualified provider to participate in the program to serve enrollees. States have the right to determine who is a “qualified” provider and some have tried to disqualify Planned Parenthood because they provide abortion services. While Congress was voting on the 2025 Budget Reconciliation Law, the Supreme Court issued a ruling in Medina v. Planned Parenthood South Atlantic, and gave states that oppose abortion more latitude to disqualify Planned Parenthood clinics from their network of Medicaid participating providers. Regardless of the outcome of the cases challenging the provisions of the 2025 Budget Reconciliation Law, the Supreme Court’s ruling on Medina will mean that states will be able to act on their own to block their state from including Planned Parenthood as a Medicaid provider.
Over the past decade, at least 14 states have sought to ban Planned Parenthood clinics from qualifying for reimbursement in their Medicaid programs. When Texas excluded Planned Parenthood from participating in their state-funded family planning program in 2013, fewer people received contraception, there was a reduction in the rate of contraceptive continuation, and an increase in the share of childbirth covered by Medicaid. While Planned Parenthood clinics make up a relatively small share of the reproductive health safety net, they serve one third of all patients that obtain contraceptive care from publicly supported clinics (Figure 4). In some communities, this loss could leave residents without a source of reproductive care.
The loss of Planned Parenthood clinics through Medicaid means that there could be fewer providers available to serve women, especially in some rural or medically underserved communities. According to Planned Parenthood, 76% of their clinics are located in rural or medically underserved areas and excluding them from the Medicaid program could force clinic closures or cutbacks in care for these populations.
The Role of Title X
Over the last few years, the Title X program, which has been providing assistance with family planning costs to clinics that serve low-income individuals since 1970, has been the focus of significant restrictions that have made it difficult for many clinics to continue to participate in the program. Title X distributes grant funds to support family planning services to low-income and uninsured people through a network of participating clinics. These services include contraceptive care, STI screening, and preventive cancer screenings, like Pap smears and breast exams. The types of sites that rely on this support include Federally Qualified Health Centers, state and local health departments, school-based clinics, independent clinics, hospital outpatient departments, and currently some Planned Parenthood clinics.
During the first Trump Administration, HHS changed the Title X regulations so that clinics that offered abortion referrals or that had co-located abortion services were disqualified from participating in the program. Others left voluntarily because they felt that this policy violated their mission and values. Approximately 1,000 clinics, including over 400 Planned Parenthood clinics across the country, stopped receiving Federal Title X support as a result of this policy. Many of the clinics later rejoined the Title X program after the Biden Administration reversed the Trump Administration regulations, however, the Trump Administration is currently withholding Title X funds from 12 grantees since April 1, 2025, affecting close to 300 clinics (Figure 5).
While the administration has not yet moved to change the Biden era regulations, they may still reinstate the restrictions of the first Trump Administration if the program continues to exist. This was a priority that was highlighted by the authors of Project 2025. Title X Clinics that lost their funding in 2025 have already had to make difficult decisions about reducing services, laying off staff, or potentially closing their doors. Planned Parenthood has already announced the closure of at least 32 clinics this year spread across California, Illinois, Indiana, Iowa, Michigan, Minnesota, New York, Ohio, Texas, Utah, and Vermont. Utah and Vermont’s entire Title X networks are comprised of exclusively Planned Parenthood clinics, so as these clinics close or lose Title X and Medicaid funding, women in Utah and Vermont may find it difficult to find another provider that offers the range of care they have been receiving at no or low cost. Two of Vermont’s Title X funded Planned Parenthood sites are in areas that do not have any other nearby publicly funded clinics. Many of these clinic closures are also occurring in the Midwest, impacting many rural communities, and leaving them with fewer options to obtain low or no cost sexual and reproductive health care.
President Trump’s FY 2026 Discretionary Budget Request would eliminate the $286 million appropriated for Title X for 2026. The Republican-sponsored House Appropriations FY 2025 Labor-HHS bill was approved by the Appropriations Committee in July 2024 and would have eliminated all support for the Title X program. There is uncertainty as to whether Congress will pass a budget this year or simply pass a continuing resolution that carries forward existing funding levels for government programs. In 2023, the Title X program administered funds to 3,744 clinics that served 2.8 million clients.
Federally Qualified Health Centers
As Planned Parenthood and Title X clinics are under threat and face closure or service reductions, a common argument by abortion opponents is that federally qualified health centers (FQHCs) will be able to fill in the gaps. FQHCs are funded under Section 330 of the Public Health Service Act and rely heavily on Medicaid payments for services. FQHCs comprise an extensive national network of more than 16,000 service sites across the U.S. They are located in medically underserved urban and rural communities and provide a range of medical, behavioral, and supportive services to all patients regardless of their ability to pay.
By law, FQHC networks are required to provide “voluntary family planning services,” as part of the broad range of primary care and related services they offer. This typically includes services such as contraceptive care, testing and treatment for STIs, and pregnancy options counseling. However, not all clinics within an FQHC network necessarily offer family planning services, and among those that do, many do not offer their patients the full range of contraceptive methods (Figure 6). It is unlikely that FQHCs could make up for the loss of services from Planned Parenthood and expand to serve more patients, especially in the face of significant revenue losses that will result from the reduction in the share of patients with Medicaid and the growth in uninsured that are spurred by the 2025 Budget Reconciliation Law.
Additionally, the Trump Administration recently announced that programs that are deemed federal “public benefits” are barred from serving individuals who are undocumented. This includes Title X and health centers. As a result, clinics receiving Title X and Section 330 funds may be denied these funds if they do not verify immigration status for the patients they serve. This is in conflict with federal law that requires community health clinics to serve patients regardless of immigration status, so questions remain about how this new limitation will be implemented.
Indian Health Service and Rural Health Clinics
Indian Health Service (IHS) clinics and Rural Health Clinics are also part of the reproductive health safety net that provides contraceptives and will likely be affected by cuts to Medicaid. IHS, an agency under the Department of Health and Human Services, provides a wide range of federal health services to approximately 2.8 million American Indian and Alaska Native (AIAN) individuals via a network of hospitals, clinics and health stations. Federal regulations require IHS to cover health promotion and disease prevention services, which include family planning services and STI services. However, the availability of contraceptive methods varies by clinic. While services at IHS and tribal clinics are provided with no cost-sharing, services are generally only available to members or descendants of members of federally recognized Tribes who live on or near federal reservations. An estimated 70% of revenues generated by reimbursements come from Medicaid. Given projected growth in the uninsured due to the 2025 Budget Reconciliation Law, IHS facilities could have fewer resources to cover the costs of the reproductive health care they provide to Native American communities.
Clinics that are part of the Rural Health Clinic program are certified by the Centers for Medicare & Medicaid Services (CMS) because they are located in rural areas designated as shortage areas and are required to provide primary and preventive care and basic laboratory services. Rural Health Clinics consist of a network of about 4,500 clinics and receive enhanced reimbursement rates for services provided to Medicaid and Medicare patients. Rural Health Clinics can provide contraceptives, but like IHS clinics, the extent of contraceptive services that are provided varies by clinic and state. The ban on federal Medicaid payments to Planned Parenthood clinics could also put pressure on Rural Health Clinics in certain locations to provide additional reproductive health care services, particularly for women who live in rural communities that have been historically served by Planned Parenthood.
